03/15/2019
A good night’s rest benefits mental and physical health. The body’s normal healing and restoration processes during sleep are crucial for recovery, particularly after brain injury. With one-third of American adults not getting the recommended seven hours of shut-eye each night, it’s valuable for treatment teams to understand sleep and its positive impact (1,2).
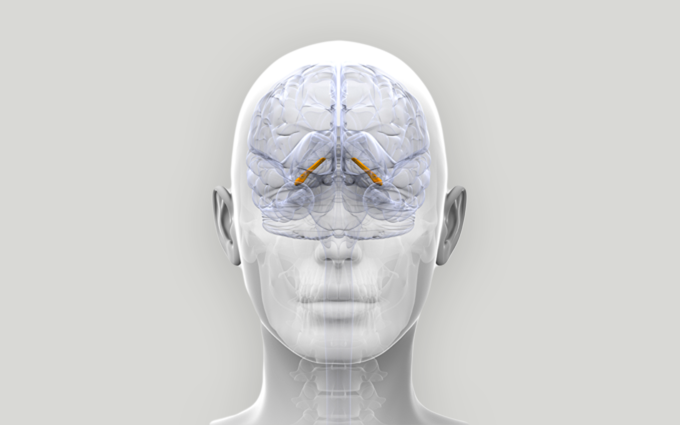
Sufficient sleep supports physical and mental health, cognitive and immune functions. Let’s look at how sleep impacts the brain. Neurogenesis – the birth and maturation of neurons – takes place in the hippocampus and plays important roles in memory functions, mood, and sleep.
The hippocampus is vulnerable to brain trauma, and sleep deprivation adds insult to brain injury because of a decline in neurogenesis. We also know that a newly discovered cellular-waste removal system called the glymphatic system clears toxins from the brain during sleep.
Aerobic exercise promotes sleep and improves mood and cognitive functioning, probably also because of neurogenesis. On the other hand, excessive alcohol use, lack of physical activity, and various stressors contribute to sleep disturbances.
High quality sleep is important for everyone, but especially for people with brain injuries. Brain injuries may cause difficulty falling asleep, an inability to stay asleep for the necessary number of hours, or excessive daytime sleepiness.
A brain injury can also cause sleep disordered breathing or sleep apnea. Other causes of sleep apnea include:
• large neck circumference
• excessive weight
• an overbite
• narrow airway
Risk factors for sleep disorders include:
• cardiovascular disease
• hypertension
• diabetes mellitus
• smoking
Sleep apnea usually requires airway pressure therapies such as continuous positive airway pressure (CPAP) or custom oral devices, and surgery may be advised in rare cases.
Circadian rhythm sleep-wake disorders can occur as a consequence of a brain injury. Circadian rhythms are 24-hour clock cycles that influence physical and mental processes and behaviors. The environment — especially light and darkness, eating, or exercising — influence these rhythms.
Some people with brain injuries experience sleep problems because of headaches or other painful conditions. When people have frequent nightmares after an injury, they may have anxiety, depression, or post-traumatic stress disorder. Interrelationships among brain injury symptoms can mean the causes might be complicated.
Sleep disturbances can affect mood, make painful conditions worse, and cause cognitive problems. Cognitive problems can cause anxiety, and anxiety leads to sleep problems.
People with brain injuries may go on to have chronic insomnia (lasting more than three months). Early evaluation and treatment of sleep disturbances, and these associated problems, can prevent intractable patterns from developing. It turns out that sleep medications are not the best treatment for anyone with a sleep problem, although they are often a first choice.
Medications, including over-the-counter medications, can actually contribute to sleep problems. Drugs that affect memory or other cognitive functions should be avoided. Over-the-counter melatonin and ramelteon, a medication similar to melatonin, can be a short-term treatment for insomnia, but these agents should not be used on a chronic, daily basis. They can interfere with other medications such as anti-depressants, and should not be taken by anyone with a seizure disorder.
Cognitive Behavioral Therapy (CBT) uses a range of strategies to promote sleep stability and may be a better approach than medications. CBT includes a series of sleep assessments and advice. A sleep diary is helpful for documenting sleep patterns and behaviors. Sleep hygiene refers to activities that promote a good sleeping pattern. One example is avoiding caffeine after the morning hours.
Maintaining regular sleep-wake and meal times (sleep stability) can regularize sleep patterns and prevent insomnia. Naps may help people with brain injuries in the early stages of recovery if daytime sleep does not interfere with nighttime sleep.
Doing something relaxing like reading or listening to relaxation tapes before bedtime can promote sleep. The bedroom should be safe, dark, quiet, and comfortable, and the bed should only be used for sleep and intimacy.
Exposure to natural sunlight or short-wave (blue) light during the day can promote a good sleep pattern, but these forms of light are not conducive to sleep at night. Artificial light from electronic devices and LED lights is usually blue light. These types of light inhibit both secretion of the body’s natural melatonin and delta brain waves that promote sleep. A warm light mode on devices can promote sleep.
Sleep masks and earplugs may help if disturbing environmental conditions can’t be altered.
Shift work disrupts workers’ sleep-wake cycles, especially if the shifts change frequently or do not match a person’s preferred sleep pattern. Police and firefighters, first responders, and truckers, and healthcare workers are at increased risk for sleep deprivation, and worker injuries can result.
Any work outside the interval of 7 a.m. to 6 p.m. is linked to poorer sleep and circadian-sleep disturbances. The CDC’s National Institute for Occupational Safety and Health (NIOSH) recommends regular rest of ten consecutive hours per day off-duty, and rest breaks every one to two hours during demanding work. NIOSH recommends five eight-hour shifts or four ten-hour shifts weekly. Night shifts of no longer than eight hours are best (3).
NIOSH recommends one to two days off-schedule after each of these weekly shifts. For shift workers with brain injuries, schedules may need to be modified to facilitate recovery and to prevent another injury.
A comprehensive approach to evaluation and treatment of sleep problems can be extremely helpful in promoting optimal outcomes for those with a brain injury. The unknown Irish author of this quote might be right: “A good laugh and a long sleep are the best cures in the doctor’s book.”
(1) How Much Sleep Do I Need?. https://www.cdc.gov/sleep/about_sleep/how_much_sleep.htmL
(2) CDC – Sleep Home Page – Sleep and Sleep Disorders. https://www.cdc.gov/sleep/index.html
(3) Sleep | Blogs | CDC. https://blogs.cdc.gov/niosh-science-blog/category/sleep/
Stay up to date with industry news by connecting with Paradigm on LinkedIn, Twitter, and Facebook.